Transparency Tools Work — but Require Appropriate Incentives
A recent New York Times article by Reed Abelson blames the slow adoption of online transparency tools on “health care’s complexity.” Abelson argues… “It is impossible to know, for example, whether a dermatologist who costs twice as much as another can more successfully diagnose skin cancer.” The article briefly mentions the case study of two large employers who found online transparency tools did not reduce consumer spending.
Abelson conveys a rather disparaging message. According to Abelson, transparency tools are mostly ineffective at reducing health care spending because patients aren’t using them. Abelson interviewed Mitch Rothschild, executive chairman of the transparency firm, Vitals. I’ve met Rothschild and co-presented with him on a panel discussion at a conference. Rothschild observed, “You can’t save money if people aren’t shopping.” That’s a good point. How can employers encourage workers to use the tools? It requires the appropriate application of training – and incentives.
I’m reminded of an experiment by the California Public Employee Retiree System (CalPERS) conducted by the insurer, WellPoint. Charges for hip and knee replacements vary considerable from one hospital to the next for no apparent reason — other than the fact that most patients have little reason to compare prices. A surgery that costs $70,000 at one hospital may only cost half that at another hospital. California health insurer WellPoint (now Anthem) observed that hospital charges for joint replacement ranged from $15,000 to $110,000 with little difference in outcomes between high-cost and low-cost surgeries. Although prices varied among hospitals, dozens of California hospitals charge less than $30,000 with no discernible reduction in quality.
CalPERS and WellPoint designed an experiment to reward beneficiaries who patronized high-quality, lower cost facilities. Enrollees were encouraged to go to the lower-priced hospitals through reduced cost-sharing. This was not a restrictive network; patients could go anywhere. But patients were responsible for all charges in excess of the $30,000 reference price for a hip or knee replacement. In addition, enrollees faced a standard coinsurance percentage of 20 percent of the cost of care (limited to $3,000 annually). This meant that choosing a more expensive hospital that charged $40,000 would subject a patient to cost-sharing of $13,000 ($10,000+$3,000). By contrast, selecting a facility that only charged the reference price of $30,000 would result in cost-sharing of $3,000.
The results of this experiment were better than anyone could have anticipated. CalPERS enrollees who went to the 46 reference price hospitals (those charging less than $30,000) are represented by the solid red bars in the figure. The solid blue bars represents the additional cost for CalPERS’ enrollees who chose a hospital other than one of the 46 value hospitals.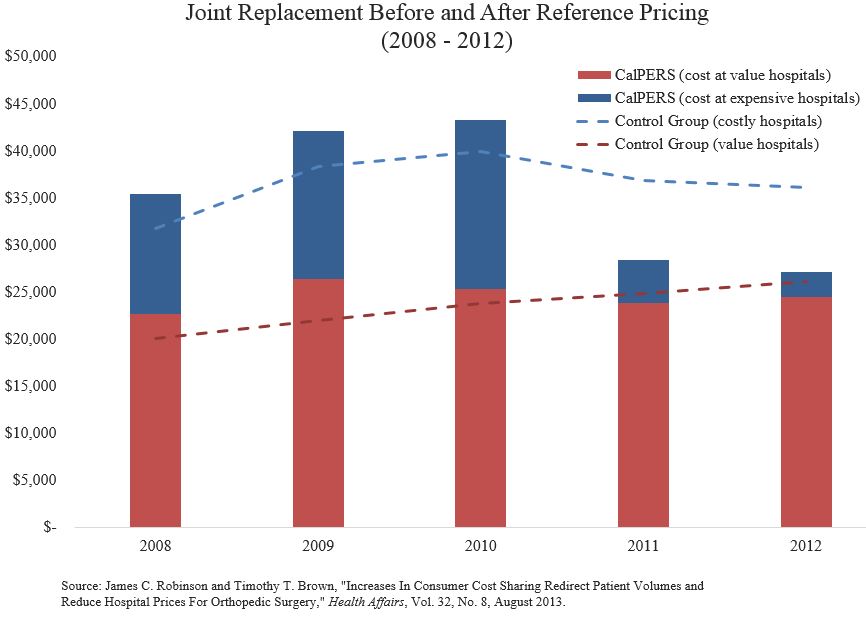
Prior to the beginning of the experiment, surgeries at a nonreference price hospitals cost far more than surgeries at reference price hospitals. For instance, in 2008 the nonreference price hospitals that treated CalPERS enrollees charged $12,821 more, on average, than the 46 reference-priced hospitals for the similar patients. In 2010, the premium CalPERS paid per surgery for enrollees arbitrarily choosing the expensive hospitals was $17,984 more. After the experiment began in 2010, the volume of CalPERS enrollees having joint replacements at high-cost facilities fell by more than one-third. However, within a year after the experiment began, it hardly mattered where CalPERS enrollees sought care. Competition for CalPERS members’ patronage drove down the price at the formerly expensive hospitals 34 percent, as the hospitals that had previously charged CalPERS enrollees more began to match the reference price. By 2012, the nonreference (high-cost) hospitals only charged $2,621 more than the value hospitals. An added bonus was that even the low-cost value hospitals lowered their prices ― by nearly 6 percent.
Notice the dashed red and blue lines in the figure. These represent a control group of Anthem enrollees who were not CalPERS beneficiaries. Prior to the experiment, the control group had similar surgical costs compared to CalPERS enrollees. Two years after the experiment began the surgical costs for members of the control group being cared for at the higher-cost hospitals was much higher than for CalPERS members. For instance, Anthem’s costs for surgeries at high-cost hospitals were $9,935 higher than surgeries at low-cost hospitals.
I have shopped around for better deals on prescription drugs. I have searched for lower-cost MRIs and CT scans. My wife and I have both used convenient labs were prices are low and transparent. We did this because I knew it was possible and our health plan deductibles are high. I don’t believe we are any different that other consumers when faced with the prospect to wasting hundreds of dollars on medical services that are unnecessarily overpriced. That’s why training and incentives are both so important. People are less likely to use tools they don’t know how to use and don’t perceive a need for.


Great article, thanks.
Of course Calpers has many thousands or even millions of subscribers, which would cause all hospitals to become more competitive.
I would love to hear any ideas for creating the same pressure on providers from the multitude of much smaller insurers around the country.
I have always favored a national fee schedule for hospitals.Your example might be a way to get there without heavy handed and (most likely) ineffective dictates from the federal govt.
“I have always favored a fee schedual for hospitals”
What a liberal idea!
How about we let the free market set price? Why are insurance companies paying the doctor and hospitals? All benifits should be payed to the insured , after all the insured payed the premiums.
Abelson argues… “It is impossible to know, for example, whether a dermatologist who costs twice as much as another can more successfully diagnose skin cancer.”
Faced with imperfect information, a patient rationally acts on the information he has. To pay twice as much for what’s apparently an identical product is to play the fool.
The case of insurance is special, however, since anyone who participates in the insurance game, like one who plays roulette, has already shown himself to be a fool. Indeed, roulette makes more sense. If you bet your annual insurance premium on a single spin of the roulette wheel, you will gain an expected return of 95 cents compared with the 80 cents or less you get in healthcare value from Obamacare or other types of health insurance.
Devon you could not be more wrong insisting that more competition is better throughout the healthcare spectrum. This was testimony given in front of the SBA and congressional staff members.
Good Afternoon,
My name is Michael McDonald and I am President of Clinical 1 Home Medical, a Weymouth, Massachusetts based provider of home respiratory equipment, hospital beds, power wheelchairs and other items of durable medical equipment. Clinical 1 has been in business for 17 years, serving patients in the Greater Boston, Worcester and Cape Cod markets.
I appreciate the opportunity to speak to the members of the Small Business Administration today. This forum will give me and others the ability to relay to the SBA just how dangerous and reckless CMS has become. To say that patients’ lives have been put in jeopardy by reckless Medicare policy is not an exaggeration. We have all heard loud and clear just how bad the VA system is in relation to the treatment of patients. I am here today to tell you that due to CMS’s implementation of competitive bidding, capped rentals on home oxygen therapy and ongoing unnecessary audits, the issues that Medicare patients face as it relates to their receiving proper home medical equipment and repairs is as bad if not worse than what is going on with the VA.
Clinical 1 was awarded contracts in the first round of competitive bidding. Some use the word “won” but I have never used the word “won” as it relates to the contracts. Competitive Bidding has been nothing short of a complete disaster for our company since July 1, 2013. Unfortunately for patients in the Boston MSA, Clinical 1 is one of only 5 local companies that has the ability to deliver the contracted products. Most of the other 20 or so companies are outside the Boston MSA with many companies located hundreds if not thousands of miles away. We take pride in providing same day delivery to Boston area hospitals. How in the world is a company located in Florida going to deliver a portable oxygen cylinder to Massachusetts General Hospital on a Friday afternoon so that the patient can be promptly discharged? How is that same company in Florida going to service the patient when at 2:00 a.m. the oxygen concentrator breaks down? Due to the fact that so many companies from outside of the Boston MSA were awarded contracts the 5 companies who are left are completely overwhelmed and unable to keep up with demand. Clinical 1 which had a stellar reputation in the Greater Boston area has seen its reputation tarnished simply because we cannot possibly satisfy the needs of the thousands of Medicare recipients who are looking for equipment. Unfortunately, due to the reimbursement rates (which are 15% less than what we bid yet we were still awarded contracts) we were and are unable to hire any additional employees. I wonder if CMS when boasting about the savings of the program takes into account the federal dollars spent with hundreds if not thousands of companies filing for bankruptcy and the thousands of employees filing for unemployment benefits along with the thousands of unnecessary overnight stays in the hospital that have cost the American taxpayer millions and millions of dollars.
Time and time again we are told by case managers that they simply cannot get equipment for patients who are looking to go home. Currently Clinical 1 is telling patients and case managers that we are three weeks behind in being able to deliver and set up a home hospital bed. The other providers in the Boston MSA are telling case managers and patients the same time frame. Patients by the thousands across the country are going night after night without the proper equipment. Just last week we had a case manager from a major Boston teaching hospital tell us that they had to keep a COPD patient at the hospital for an additional 4 nights because they were not able to get a hospital bed, wheelchair and low air loss mattress delivered to the patient’s home because there was no provider who could take the patient. Of course that same case manager could have called the company located in Tennessee who was awarded a CMS contract in the Boston metro area to have the hospital bed delivered. Can you imagine being a patient who is looking forward to getting discharged from the hospital to go home to the comfy confines of their house but are unable to do so because a case manager cannot locate a bed provider due to so many local companies being forced out of business because of the bidding program?
We have hundreds and hundreds of examples of how these policies have negatively impacted the health and well-being of patients and CMS has to be held accountable for this program and the devastation it has caused patients and their families. One example that comes to mind is a patient who is a paraplegic who called our office numerous times asking us to fix her power wheelchair. Not to sound overly dramatic but I personally spoke to this patient who completely broke down on the phone when she told me that she has been unable to get off of her couch for 3 weeks because her power wheelchair is broken and there is no provider in Boston willing to help her. We are inundated with calls from patients looking for repairs of their power wheelchairs but unfortunately we have to tell the patients that we are 2 to 3 months behind in being able to provide repairs for chairs that other companies have provided to these patients but have since gone out of business due to reckless, inexcusable CMS policy causing devastation to area small businesses. On a daily basis, Clinical 1 receives calls from customer service reps from 1-800-Medicare who are looking for providers to fix power chairs. Every so often I will instruct our CSR’s to give the call to me which allows me to ask the representative from Medicare how many calls they get regarding a patient’s inability to get repairs and or equipment. Their response each and every time is “a lot of calls”. There is the story about a Boston hospital that routinely holds orthopedic discharges for patients that need walkers. Just recently a hospital executive at that hospital told me that they held a double knee replacement patient for an extra night because they couldn’t get a $49 walker delivered. How much did that cost the tax payer? Another example that comes to mind are the 70 or so oxygen patients that we have documented who have called our office since the beginning of the year telling us that they all of a sudden do not have a provider due to their provider suddenly going out of business. There are two reasons why oxygen providers are closing their doors. One being the aforementioned bidding program and the other being a 36 month cap on the rental of home oxygen. The 36 month capping of oxygen has had a devastating effect on a patient’s ability to receive service after the 36 month cap. After the 36th month providers under current Medicare law are supposed to provide 24 hour, 365 days a year service to these patients for 2 years without the ability to bill Medicare for these services with the exception of a 6 month maintenance fee. It is simply unfair and disgraceful that small businesses are made to work for free for 2 years! Is there another industry in the country where companies are forced to provide care and or services free of charge for 2 years? It is blatantly unfair and most will say unlawful. As you can imagine, there are not too many oxygen providers that are too excited about sending a technician out at 2:00 a.m. to exchange a broken concentrator free of charge for 2 years after the cap hits.
Unfortunately CMS has not learned of their past mistakes. Just recently CMS awarded bids in multiple product categories for the next round of bidding which starts July 1, 2016. In this round there are even fewer local providers and even more providers located 1,000 miles away or more. The ineptness of CMS is inexcusable and quite frankly mind boggling. One category that blows my mind is the nebulizer category. The closest provider who is able to deliver a nebulizer to a patient in Boston is located in Alabama with other providers as far away as Puerto Rico. On a daily basis we deliver nebulizers to patients who are getting discharged from Boston area hospitals. Typically we deliver nebs to COPD or asthma patients who have had a flare-up and are in the ER. Prior to discharge the patient needs the nebulizer to go home with. Can someone please tell me how a company in Alabama is going to provide a nebulizer on a Friday night to a patient at Mass General’s ER? What is going to happen is that due to the fact that there are no companies located in Boston who are able to bill Medicare for the nebulizer the hospital is going to have to call an out of network provider who is going to charge the patient privately. Unfortunately by doing that the private pay charge opens up another whole can of worms as it relates to the nebulizer medication being covered as CMS will not cover the medication because they do not have the nebulizer as being billed to them. Also, there is not a company in Boston who is going to accept the contract anyway, as the monthly rate has been cut to around $4 per month which is capped at 13 months.
Unnecessary and unreasonable audits are crippling the industry and putting providers and small home healthcare businesses out of business by the thousands. Clinical 1 is getting tens of thousands of dollars taken back as it relates to outside auditing companies who are paid by CMS on how much they take back from providers. The companies are raking in hundreds of millions of dollars taking back money from small businesses who have provided medically necessary equipment that was ordered by a physician. These takebacks are due to the RACS, ZPICS, CERTS, etc. not being able to read a physician’s signature, or forms being in the wrong dated order or for simply no reason at all. The audits are sent in with an overwhelming amount of clinical paperwork justifying the equipment that was ordered by the physician, however because these auditing companies are again paid by the amount of money they takeback there is no clinical inference when determing the outcome of an audit or an appeal for that matter. The appeal process is so lengthy and cumbersome that you spend way more time and money fighting for the denial to be overturned that so many providers simply give up and that is exactly what Medicare wants. Not only are the small businesses losers when it comes to audits but patients lose out as well. I am ashamed to admit it but Clinical 1 has taken back hospital beds, wheelchairs, support surfaces and walkers from patients who clearly have a medical need for the products which were prescribed by a physician but cannot afford to pay for it out of pocket after one of these auditing companies has determined that it is not medically necessary. Just recently we had a standard K0001 wheelchair denied for a double amputee, diabetic patient after having submitted all of the necessary clinical documents. The reason: “Not medically necessary”.
Since the number of providers who are able to bill Medicare has been cut from the thousands to around 600 providers I wonder if CMS has laid off thousands as it would seem to me that there does not need to be the tens of thousands who are employed directly by CMS, NSC, CBIC’s, PDAC’s, auditing agencies, etc to administer and monitor the program if only 600 providers are left? I would ask the SBA to see if we can get a count as to how many people are involved in administering this program to oversee the billings of only 600 plus providers.
Lastly, as I mentioned before CMS and the architects of this program should be held accountable for their failed policies. Make no mistake about it, the bidding program and auditing programs have failed leaving small businesses and patients left to pick up the pieces. High level CMS executives have sworn under oath in front of Congress testifying at length about how patients and small businesses have not been negatively affected by this program and how the program has been an overwhelming success. We here at this hearing along with hundreds of thousands of patients, physicians, case managers and providers across this country know differently. The time has come for Congress to launch an investigation into the harmful and devastating effects of this program.
I thank you for taking the time today to listen to my testimony.
Michael McDonald
Final copy
This statement says CMS is the problem, not “competition”.
And that’s not exactly news.
Micheal Douglas, don’t worry because help is on the way:
“The US Department of Health and Human Services and the Cuban government on Monday signed a memorandum of understanding to encourage cooperation between the two countries on health matters…Cuba has made significant contributions to health and science,” HHS Secretary Sylvia Mathews Burwell said in a statement. “This new collaboration is a historic opportunity for two nations to build on each other’s knowledge and experience, and benefit biomedical research and public health at large.”
It will be much cheaper when we need to get a $49 walker to a Boston hospital when it comes from CUBA instead of Tampa Bay. Maybe these Boston hospitals could have a couple of those $49 walkers on hand instead of getting one at a time from you.
When these old women need their wheel chair fixed, why don’t they pay for it? Must the bucks come from Medicare?
Senator, Micheal Douglas must have given his testimony before the other Congress. 😎
Friday NewsFlash: Minnesota’s largest health insurer, Blue Cross and Blue Shield of Minnesota has decided to stop selling health plans to individuals and families in Minnesota starting next year.
Obamacare killing Individual Medical (IM) Insurance. This was the goal so everything is perfect for Democrats and Hillary.
If they moved the top counties of IA into MN it would double the IQ of both states!
http://townhall.com/tipsheet/guybenson/2016/06/24/its-working-blue-cross-plan-exits-obamacare-gop-rolls-out-replacement-proposal-n2183088
Ron,
Everyone knows this is Bushes fault. If he wouldn’t have lost to Bill in 92 we would have never heard of the Clintons again. I blame George H for everything now.
quick note:
Blue Cross MN is still offering an HMO. What they cancelled are all the PPO plans.
And:
Thanks to Michael Mcdonald for showing the folly of trying to cover every little piece of equipment in an insurance plan. Is Medicare really taking bids on $49 items? I think that we need to raise the Part B deductible to $1500 right away, with some assistance for seniors who are poor.
“I think that we need to raise the Part B deductible to $1500 right away, with some assistance for seniors who are poor.”
Amen Bob. Throw in a $10,000 out of pocket maximum liability for Parts A and B combined and I would get rid of my supplemental plan which is costing my wife and me almost $400 per month for the two of us.
Even President Obama is in favor of doing away with some of the Medigap policies that have first dollar coverage. Those with the most generous Medigap plans spend something like 30% more when controlling for health status.