Repeal and Replace
On this first anniversary of the president signing the health reform bill into law, Investor’s Business Daily features an editorial I wrote with Newt Gingrich and Jim C. Capretta. It reflects our one-year assessment of ObamaCare that we presented to the National Press Club last week:
- Ever-More-Costly Mandate: ObamaCare will force Americans to buy insurance whose premiums will rise at twice the rate of their incomes.
- Bizarre System of Subsidies: Depending on where insurance is bought, the subsidies for individuals are radically different, a cost factor so large it will force a major reorganization of American business.
- Perverse Incentives for Insurers: Health plans will try to attract the healthy and avoid the sick; and after enrollment, they will over-provide to the healthy and under-provide to the sick.
- Perverse Incentives for People Buying Insurance: With small (and maybe unenforced fines), people will have an incentive to wait until they are sick to buy insurance, and then drop coverage after their medical bills are paid.
- Tattered Safety Net: With 32 million newly insured and more generous coverage for almost everyone else, there will be a huge increase in the demand for care; but the legislation has no provisions to increase supply. The result: increased waiting times at the emergency rooms and in doctors’ offices — with those whose plans pay below market being pushed to the rear of the waiting lines.
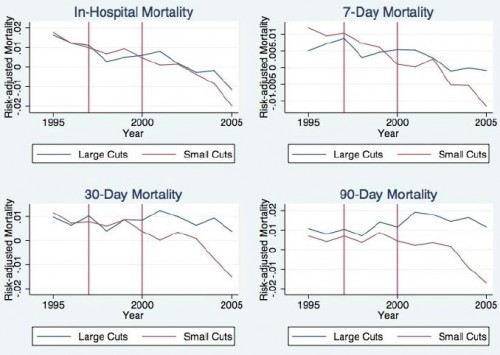
- Benefits Cuts for Seniors: Deep Medicare cuts will make it increasingly hard for seniors to find doctors to treat them and facilities who will admit them.
These problems and the recommended solutions build on a continuing consensus among critics about what the problems are and how to solve them — beginning with an editorial Newt and I wrote for The Wall Street Journal last year and a Capitol Hill think tank briefing in January with the Heritage Foundation, the American Enterprise Institute, the Cato Institute and the American Action Forum — featuring this summary document.