Pay for Performance Doesn’t Work
Health Affairs has published an important new study [gated but shows abstract] on Pay for Performance (P4P) that concludes it has had virtually no impact on physician practice. That is not to say physician practice isn't improving with time, but P4P programs have little to do with it.
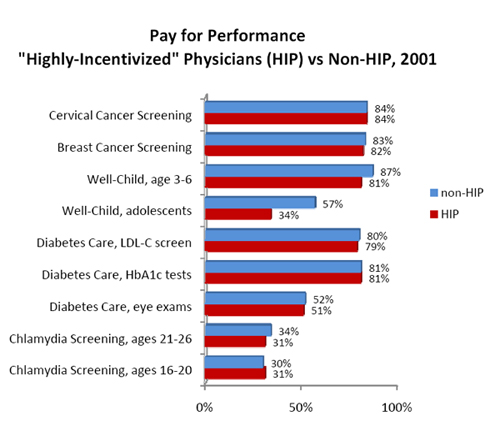
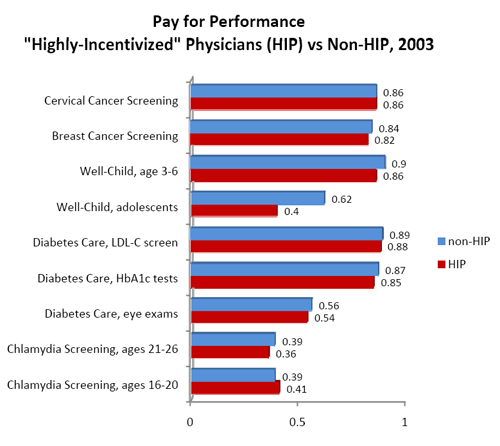
The study looks at 5,350 physicians in 154 physician groups in Massachusetts from 2001 through 2003. Overall, about half of these physicians were in P4P programs established by five health plans that cover four million enrollees in that state. The plans reported information about physician compliance with thirteen measures of performance known as HEDIS measures established by the National Committee for Quality Assurance. It compared physicians who were "highly incentivized" by P4P bonuses to physicians who were not involved in P4P programs.
Leaving aside the question about whether any of this measures anything meaningful other than marking off boxes on a check list (notice there is nothing here about actually listening to your patient, finding and treating anything that might be wrong, or persuading the patient to change behavior), what else does it show us?
It shows us that the much vaunted pay-for-performance system is useless, notwithstanding the fact that private payers, Medicare, and the presidential candidates all promise that such programs will save the health care system. In fact, on many measures the "non-incentivized" physicians improved more than those who were "highly incentivized." Golly, is it possible that physicians actually pay attention to the emerging literature and freely change their practices in the interests of good patient care? Oh, no, that can't be it.


These reforms do not work because they originate from the demand side of the market. In every other market, repackaging and repricing originates on the supply side.
Telling doctors how to practice medicine is not a solution. Allowing doctors to improve their product and profit form doing so is a solution.