Patient “Activation” in the Spin Cycle — Professors, Scams, and Conflicts of Interest
(Fowles, et al. Journal of Patient Education and Counseling, 2009)
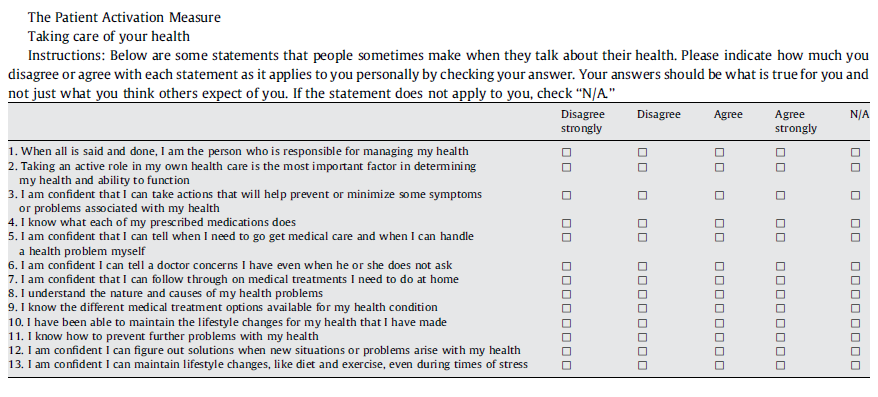
If you “strongly agree” with most of the questions above, you are a “highly activated,” patient. According to an article in the Wall Street Journal, health researchers have determined that the Patient Activation Measure (PAM) can identify “highly activated” patients, and that “highly activated patients” have better outcomes. (A New Vital Sign to Gauge: The Patient’s “Activation” Level, p. D1).
Judith Hibbard, identified as lead developer of the PAM assessment and a senior researcher at the University of Oregon’s Health Policy Research Group, assured the article’s author that the PAM is more than just a non-stick cooking spray: “Everyone assumes this is sort of a soft science, but we can measure patient activation just as rigorously and scientifically as other things in health care,” she reportedly said.
If that’s the case, health care is in bad shape.
The pilot PAM was “rigorously” developed from a convenience sample of 100 people who answered a newspaper advertisement and were paid for answering a variety of questions. It was tested on a convenience sample of 486 people who were a mix of cardiac rehabilitation patients and employees of a “large health system.” Testing with “a national sample,” was done on a random sample of 1,515 people contacted by telephone (2004). The data section merely says that a “48 percent response rate was achieved.” It was also tested on a sample of 300+ people in two companies (2009 and 2012).
In one paper, Professor Hibbard and her co-authors tested whether Chronic Disease Self-Management Program workshops led by “two trained leaders” helped “activate” patients. They recruited from a list of 8,796 people, eventually ending up with 479 people activated enough to actually participate.
Sadly, they found that there was no difference between activation in the treatment and control group. In search of silver linings they point out that
…for a few behaviors the control group showed greater gains in self-management as compared with the intervention group over the course of the study. Why this should have occurred is not clear. The findings do suggest, however, that rather than a failure in the intervention, something stimulated change in the control group over the study period. (Health Services Research, 2007)
What is clear is that more “activated” patients also tend to be married and have higher incomes and more education. In study after study, activated or not, people like this tend to be in better health.
According to the disclosure statement in a paper published in 2010, Professor Hibbard consults for Insignia Health, LLC, and has an ownership interest in it. Insignia Health in Portland, Oregon, has the exclusive license to use PAM. It assures people that Professor Hibbard and other researchers have used PAM in “hundreds” of studies, and that clients report annualized savings of $260 to $3,700 per patient.


Of course people who have higher incomes and more education are more actively involved in managing their health. They have the time, knowledge, and resources to do so.
Active engagement, or “activation,” for all of life’s concerns is finite. There are only so many hours in the day, and so much energy in the body. Being proactive about one’s health is one imperative competing with lots of others. It shouldn’t surprise anyone that people struggling more in other categories would have less attention to devote to health concerns.
I’m not clear on how this measure results in monetary savings…?
I agree, Diane. I would think that Patient Activation Measures would cause them to go to the doctor more often, resulting in more costs.
Perhaps it’s because PAM really allows people to get help before their condition becomes more serious. If someone who didn’t follow PAM let their condition get out of hand because they didn’t think that they needed to go see a doctor, then it would cost them more to restore them to health.
…more “activated” patients also tend to be married and have higher incomes and more education. …tend to be in better health.
That’s one of the problems public health advocates run into when they attempt to reduce health disparities. Whether you call it patient activation, patient education, chronic disease management, or health & wellness, it’s tough to get a positive change in your dependent variable “Y=health status” given a standard input of the treatment “X” across groups. There are generally intervening variables (e.g. marital status, incomes and education).
I can testify that marriage is an important factor, probably interacting with education and income. The spouse is usually the real primary-care practitioner!
As any doctor will tell you, many middle-aged men wait to see a doctor until their wife makes them go. My significant other has threatened to have her assistant put my annual medical checkups on a “preventative maintenance” schedule. That way she has a reminder to make my appointment (and make me go).
It seems as if most of this stuff is common sense. Obviously those who “agree strongly” that they are responsible for their health and know when to get help are going to be healthier because they have a better gauge. Additionally, this knowledge to know when something is wrong comes from being more educated. So, I don’t think there is causation, but rather correlation.