Austin Frakt and I Agree on Something
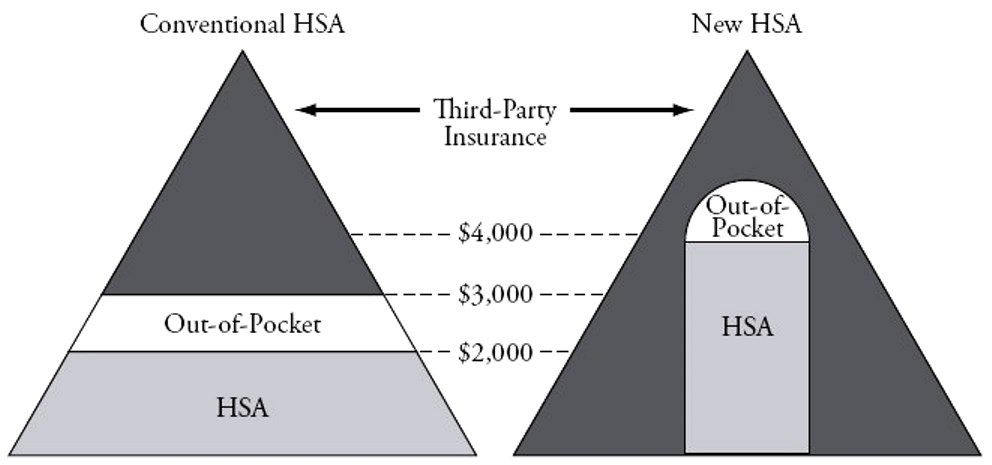
Across-the-board deductibles don’t make a lot of sense. In Priceless, I argued that whole categories of care should be transferred to the patient in some cases and there should be first-dollar coverage for other kinds of services. Austin Frakt seems to agree, reproducing this graph from the book, and remarking:
LASIK is an elective procedure, the purpose of which is well understood by the patient. I’m on board with the idea that insurance shouldn’t cover such things, or if it does, not the full cost and certainly not the marginal cost. All health procedures just like this are good candidates for the purview of John Goodman’s “New HSA.”
The issue is not whether the procedure is like LASIK surgery, however. The issue is whether choices by the individual will create costs for other members of the insurance pool. Where there are no “financial externalities,” the case for individual decision-making is strong.


I agree with the premise behind allowing individuals to create costs. After all, there are services that require some form insurance in cases of expensive and prolonged care, but there are many cases that don’t and therefore prices should be adjusted according to demand for these services and not altered by the middle-man.
Interesting. I really hope that the fundamental way our health care system works changes toward empowering the patient/consumer like other industries do.
You make an excellent point here, and I agree with both Austin Frakt and Dr. Goodman. It’s important to make a big emphasis on the fact that individual choices shouldn’t represent an increase in costs for the rest of people in that insurance pool. That’s the foundation for maintaining a fair system that doesn’t overcharge/undercharge anyone.
Very clever! Health Savings Accounts are an excellent approach to grant individuals more options if they need access to certain procedures that are not covered under their insurance plan.
Frakt makes a good point at the end of the post by asking these questions: “What makes something elective? Does it have to be life saving to be non-elective? What makes its purpose clear to the patient? Does the patient need to understand all the risks and alternatives?” Everyone should ask themselves these same questions when arguing whether it’s fair or not that certain people have a specific coverage or not. I believe, and this is just my personal opinion, that for a procedure to be elective it has to be a matter of urgency. Meaning, the patient is in critical danger without the procedure done, and also, if it significantly improves the quality of life of that person. I’m not talking about how that person feel about themselves of whether they are happier with themselves once the procedure is done. I’m talking more in terms of quality. If it does improve the way that a person lives, then I think it’s well worth it…isn’t it?
This is very interesting. I always wonder, when do you draw the line as to what’s acceptable and what’s not in terms of coverage? I’ve always struggled to understand who determines whether a patient is allow to go through with a certain procedure and who isn’t, and how this is determined. This can be very subjective, I think.
HSAs are a very viable solution. John Goodman clearly explains why, and Austin Frakt reinforces very valid points.
@Jonathan,
That said, would you say LASIK surgery is elective or not? I’m just curious. To some people this could be a life changing procedure, whereas to others it may be just an optional one. It varies from person to person.
What makes a procedure elective or non-elective? Who determines that? This seems like a very subjective topic, especially when insurer are involved and it’s more convenient to them to limit patients to as much care as possible. So, of course, they will find ways to find more procedures than not elective…so they don’t have to cover them. Is that enough to keep a patient from receiving coverage?
The industry calls this value-based insurance design. I think it sounds like a great idea; differential cost-sharing for various medical services depending on the amount of discretion patients have and efficacy of the treatment. I also like the idea of differential cost-sharing depending on where enrollees seek care. Those who use a preferred provider get a better deal than those who want to use the highest priced hospital in the network.
I can easily see how insurers may want to make generic medications for chronic conditions might be free. At the same time, insurers may want to have a high co-payment for prescription pain relievers like Celebrex. I’m not a fan of regulations that try to mandate cost-sharing arrangements and how insurers cover services.
I think that an independent review panel should decide necessity. A doctor will most often always say a procedure is necessary – so that the patient will elect to undergo the procedure. By the same token, the insurance company will most always sat that a procedure is unnecessary – as to avoid paying for it.
While is thing this is a good idea, I am lost on how it should be regulated.