Doctors and Patients Have a Failure to Communicate
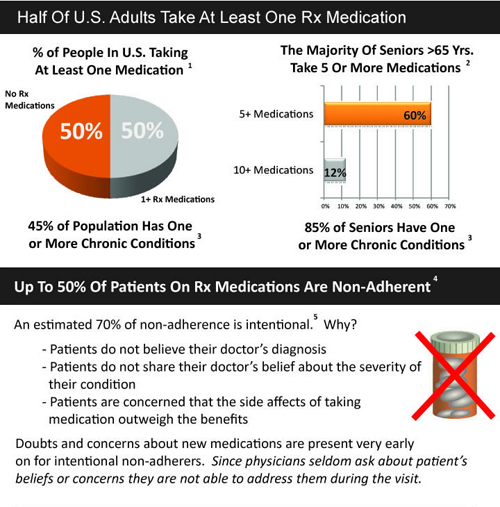
Half the U.S. population takes at least one prescription drug. Sixty percent of seniors take five or more medications. Yet, about half of patients prescribed a drug are non-adherent.
The Better Health Blog has an interesting info graphic explaining why lack of communication is a contributing factor in prescription drug non-adherence. Physicians spend only about 49 seconds during an office visit explaining to patients about their new prescription. Half of patents who leave their doctor’s office do not understand what they were told to do. Moreover, doctors underestimate the information patients need while overestimating the amount of information conveyed.


Polypharmacy is a significant issue for older adults. In addition to thesefindings, poor pill management can be associated with increase morbidity and potentially mortality.
There’s work showing that people with consumer directed policies are more adherent (even if one can believe the adherence definitions which usually consist simply of whether or not one filled a prescription, not whether or not one actually took a drug).
According to the conclusions implied here, consumer directed health insurance makes doctors spend more time explaining drugs to patients.
Why does this remind me of the claim that if physicians only spent more time explaining that smoking is bad, we’d have lots fewer smokers?
I must admit that I’m not a very compliant patient. Doctors always tend to be in a hurry when prescribing. They tend to not really listen to my issues. If I do end up going to the pharmacy, I usually balk at the list of side effects. Then again, I’ve never had to take a medication for longer than 3-4 days. I have no idea how seniors do it.
That’s about 1/3 of patients on prescriptions intentionally not adhering. I wonder if better communication could assuage these patients (or at lesat some of them), or if its still an aversion to side-effects, the “I know myself best” side of human nature, etc.
I once heard it said that the doctor pulls out his or her prescription pad as a sign the office visit is over. In addition, patients are probably more apt to feel like their time was not wasted if they get a remedy for their ailment.
However, I suspect Linda is correct that people with a CDHC plan are more adherent. This could be due to CDHC enrollees making sure they actually have a problem before visiting their doctor; or being more willing to ask questions about their prescribed treatment once there.
Public health advocates often lament that millions of dollars could be saved if people would just take their medications. I’m not entirely convinced. Once prescribed a drug, people often never question whether it’s effective or if they even need the drug. I read an article that quoted a physician about seniors who take multiple drugs. He claimed that if someone is on 12 or more drugs, the chances are half of the drugs being taken are to alleviate the side-effects of the other half of drugs. Moreover, the more drugs a senior is one, the greater the risk that some of the drugs are contraindicated.
If you want to consider another troubling possibility, consider how many patients who are enrolled in outpatient drug studies are non-compliant with the medication. I wouldn’t be surprised if it were a significant number. Hmmm…??
How to compare results of not taking the active drug versus not taking placebo?
It is always interesting to hear non medical people try to figure out what happens between a Doctor and his/her patient. The bottomline is that patients come in to the doctor expecting (and lately, demanding at times) a “quick fix” and the Doctor is pressured to provide this by not just the patient but the government, insurance company, society, etc. This is what we are trained to do is prescribe medications for various conditions. Why do patients come in for antibiotics all the time when all they have is just a cold? Same thing can be applied to imaging studies, don’t demand an MRI for your acute back pain and I won’t order one. In re: to consumer directed health insurance, I am not sure what that is but the less people we have involved between the doctor and the patient the better off we all would be.
Why wouldn’t patients want a quick fix? Would they be better off waiting for care for weeks or months as is the case in virtually all of the government run health care systems outside the US? The reason for going to a physician is to consult on the possibilities for a quick fix.
Consumer directed care usually means that the patient is paying cash for expenses up to the 1 to 5 thousand dollar mark.
Once upon a time, I was involved with Medicare+Choice, now called Medicare Advantage; i.e.,privately insured Medicare benefits. One of our chief efforts was in medication compliance. We also encouraged “brown bagging.” Having a customer bring all medications currently prescribed in a brown bag to the physician, or even better to a case manager or pharmacist, to ascertain the efficacy and possible adverse reactions. We knew that for chronic disease, Rx compliance was the best insurance against hospital admission.
CDHC does not mean acting in a void. A good plan wants to attack problems when they are treatable and avoid the costly inpatient care that results from neglect. Patient outreach is a part of these plans. I’m to the point of asking my plan not to call me suggesting I need a refill; I know I need to and can do it myself. How about you?
Some years ago, I went to a university clinic thinking I was in need of some special presciption for an inflamation issue. At the brief visit, they wrote down “Motrin” on the prescription paper. I thought to myself, “Really? I came all the way over here and paid for this?”
I felt as if I had wasted appointment time and space. It makes me wonder how many people out there have done the same thing when they could have simply done some quick research and treated themselves.
If doctors seem more rushed these days days than usual, then clinics need to consider using phone counseling more. I dunno, that may be too radical.