Tag: "Medicare"
Medical Device Manufacturers Not Paying Their Share, and Other Links
Surprise: medical device manufacturers are passing the (ObamaCare) device tax on to consumers. (The ones the president promised not to tax?)
Is immigration good for Medicare?
Another argument for buying across state lines: It appears increasingly likely that just one insurer ― Anthem BlueCross BlueShield ― will offer plans in New Hampshire’s health insurance exchange.
Medicare Advantage Lowers Costs ― for Everyone
We find that when more seniors enroll in Medicare managed care, hospital costs decline for all seniors and for commercially insured younger populations. Greater managed care penetration is not associated with fewer hospitalizations, but is associated with lower costs and shorter stays per hospitalization. These spillovers are substantial ― offsetting more than 10% of increased payments to Medicare Advantage plans.
NBER paper by Katherine Baicker, Michael Chernew, Jacob Robbins.
ER: The Gateway to Hospitalization
A RAND Health study found that hospital emergency rooms are now the point of access for nearly half of all hospital admissions in the U.S. and account for almost all of the growth in admissions between 2003 and 2009. During that time, hospital admissions grew only 4% — not even keeping pace with population growth. But ER-related admissions jumped 17%. (ModernPhysician.com)
Why this is important: about half of the newly insured under ObamaCare will get insured by Medicaid, and Medicaid patients use the emergency room twice as often as privately insured patients. Also, hospitals are buying doctors, who will be pressured to admit patients once they get to the emergency room.
One More Reason Why We Are Going to Have Physician Shortage
Here’s something by Jeff Goldsmith that I missed a few weeks ago:
We will be replacing a generation of workaholic, 70-hour-a-week baby boom physicians with Gen Y physicians with a revealed preference for 35-hour work weeks. During this same period, we’ll be adding 1.5-1.7 million net new Medicare beneficiaries a year and enfranchising perhaps 25 million newly insured folks through health reform. “Train wreck” is the right descriptor of the emerging primary care supply situation.
What about doubling physicians’ patient panels to more than 5,000?
I’ve visited real-world group practices organized this way. They reminded me of nothing so much as “I Love Lucy’s” famous chocolate factory assembly line. It was exhausting simply watching the physicians sprint through their days. You wanted to install oxygen carrels for them to catch their breath. Gen Y docs aren’t going to practice 28-slot days, with intensive “break times” to answer their emails and make phone calls. Neither are Gen Y nurse practitioners.
Headlines I Wish I Hadn’t Seen
Is the media trivializing Medicare Advantage insurance?
Congress in secret talks to exempt itself from ObamaCare.
Washington airports spared sequester impacts.
The Internal Revenue Service issued more than $11 billion in improper refunds.
Hospitals Make More Money When Things Go Wrong
A surgical complication increases a procedure’s average contribution margin by 330 percent for the privately insured and 190 percent for Medicare patients, according to a study published this week in the Journal of the American Medical Association…
When a surgical complication occurred, the profit margin jumped from $16,936 to $55,953. For Medicare patients, profits grew from $1,880 to $3,269.
HT: Sarah Kliff.
Where Does Your State Rank?
The State of Health Care Spending, by Andrew Rettenmaier and his colleagues:
The compendium is divided in two main parts. Part 1 summarizes the four ways by which the geography of health care spending is described. Health care spending as a percent of the states’ GDP is the first way in which the geography of health care is presented and is separated between Medicare, Medicaid, and non-Medicare/Medicaid spending. These data allow for analysis that extends back to 1980 for each state. Next, health care spending is analyzed on a per capita basis and is again divided between Medicare and Medicaid per enrollee in the programs, and average non-Medicare/Medicaid spending for the states’ population who are not enrolled in the programs. The second part of the compendium comprises 50 state summaries. The two-page summaries are based on the four ways of viewing geographic variation in health care spending and the health care markets. The first page summarizes the key health care spending indicators in each state, and provides graphical representations of how the state compares to the national average now and in the past. Also depicted is the variation in county level Medicare spending. The second page of each state’s summary presents all of the recent metrics in tabular form. Medicare spending in four large or geographically dispersed counties is also presented at the end of each table. (Summary by Michael Ramlet)
Tom Saving and I discuss some of the results at the Health Affairs blog.
Does Decreased Length of Hospital Stay Equal Lower Cost?
Based on a 20 percent sample of Medicare claims from 1985-2005 for people 65 and older, Brauer et al. 2009 provide data on length of hospital stay for people with hip fractures in the U.S.
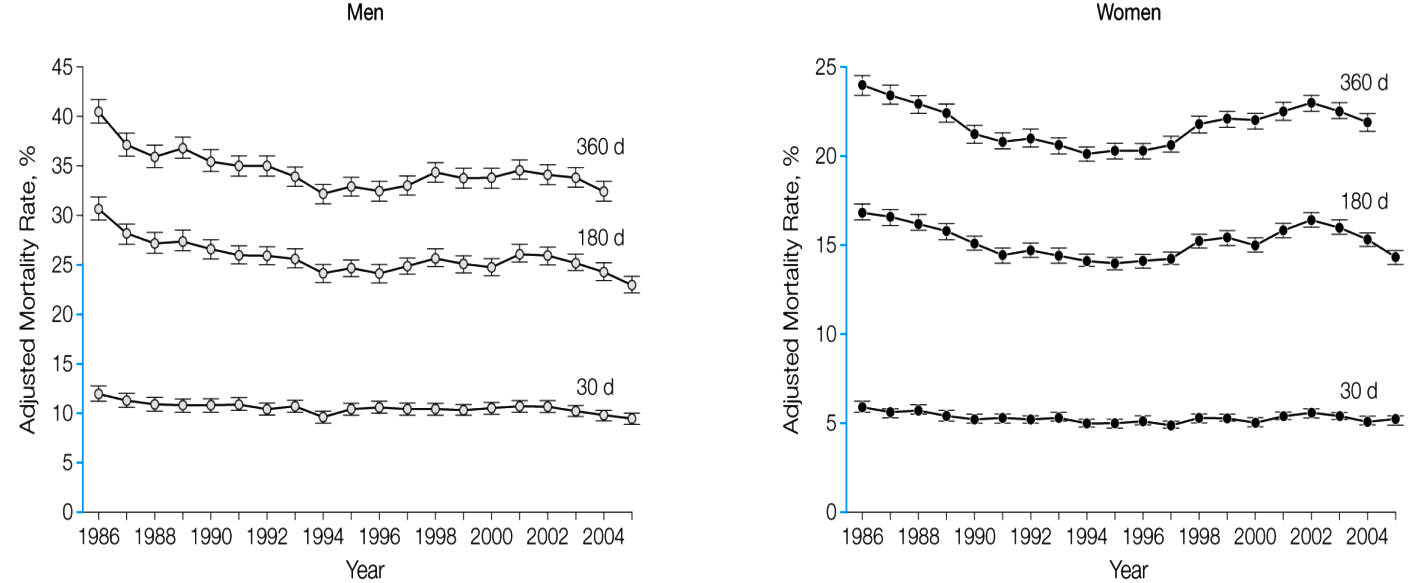
The median length of stay for hip fracture over the period decreased from 12 days to 5 days. Risk-adjusted mortality at 30, 180, and 360 days improved for both men and women:
Source: Carmen A. Brauer et al. 2009. “Incidence and Mortality of Hip Fracture in the United States,” JAMA, 302, 14, 1573-1579.
Innumerable studies in the health care literature use reduction of days in hospital as a measure of reduced costs. Unfortunately, the simple reduction of days in hospital and death rates, while welcome, tells us little about readmissions, total costs, or extent of recovery.
With the passage of DRG reimbursement in 1983, hospitals began adjusting their business models to accommodate flat rate payments. One outcome was “quicker but sicker” discharges. In 1986-88, the paper notes that 34.3 percent of hip fracture patients went home with self-care and 33 percent were discharged into skilled nursing facilities. By 2003-05, only 5.3 percent of patients were discharged home with self-care. The majority, 52.9 percent, were discharged to a skilled nursing facility.