Does Decreased Length of Hospital Stay Equal Lower Cost?
Based on a 20 percent sample of Medicare claims from 1985-2005 for people 65 and older, Brauer et al. 2009 provide data on length of hospital stay for people with hip fractures in the U.S.
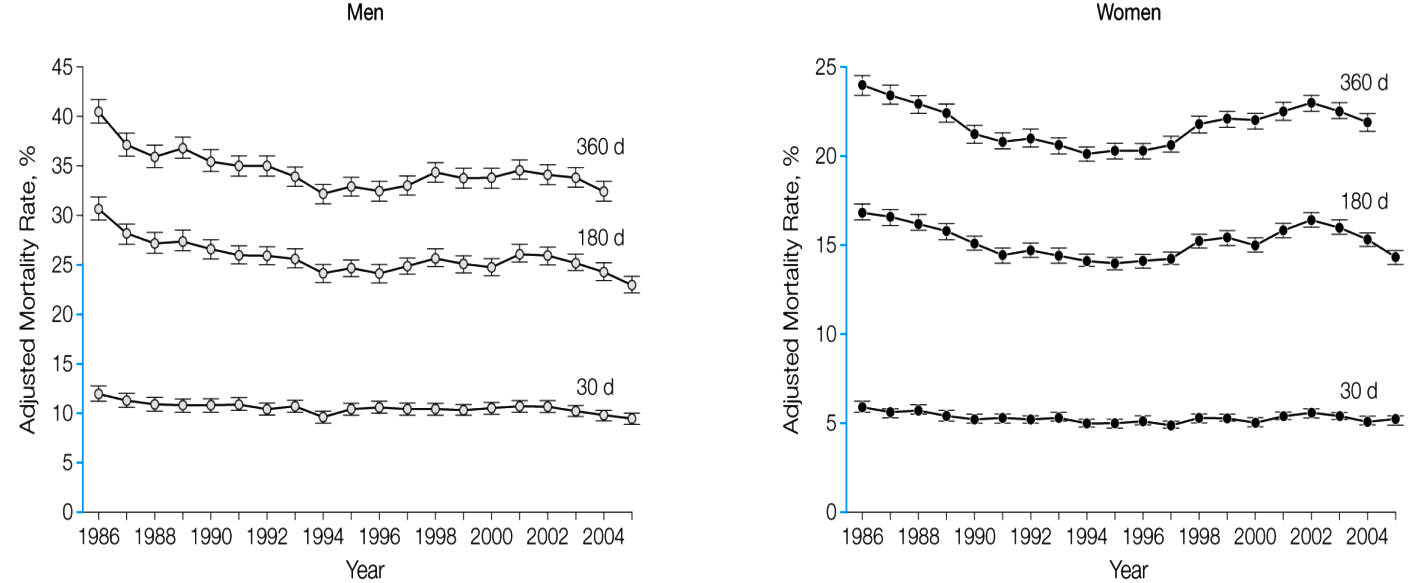
The median length of stay for hip fracture over the period decreased from 12 days to 5 days. Risk-adjusted mortality at 30, 180, and 360 days improved for both men and women:
Source: Carmen A. Brauer et al. 2009. “Incidence and Mortality of Hip Fracture in the United States,” JAMA, 302, 14, 1573-1579.
Innumerable studies in the health care literature use reduction of days in hospital as a measure of reduced costs. Unfortunately, the simple reduction of days in hospital and death rates, while welcome, tells us little about readmissions, total costs, or extent of recovery.
With the passage of DRG reimbursement in 1983, hospitals began adjusting their business models to accommodate flat rate payments. One outcome was “quicker but sicker” discharges. In 1986-88, the paper notes that 34.3 percent of hip fracture patients went home with self-care and 33 percent were discharged into skilled nursing facilities. By 2003-05, only 5.3 percent of patients were discharged home with self-care. The majority, 52.9 percent, were discharged to a skilled nursing facility.


By default, reducing length of stay means reducing days at the end of the stay. These are the least-expensive days in the hospital.
The change seems negligible for the 30d mortality rates. The study points out that most of the expenses are incurred after they leave the hospital. So are we concerned with reducing hospital costs, or reducing the cost of healthcare?
The study says that comorbidity has increased across the board. Is it evidence that DRG reimbursements = causation?
This article does well in pointing out the core problem with our health care system, which is the lack of a market-led price for consumers. As noted, price variances are artificially placed through policies that still end up affecting the patient/consumer.
Classic example of how poor intervention decisions lead to adverse effects on the patient.
I would be interested in seeing an extensive study into the demographic of people who use the emergency room and what are the reasons behind readmission.
I don’t fully understand why there is a need for readmission even after getting solid treatment. This just points out that the type of treatment patients may be getting aren’t sufficient enough or aren’t effectively addressed.
I find it interesting that the 180 and 360 day rates for women (and to a lesser extent, men) increase right after the Balanced Budget Act of 1998.