Is Fee-For-Service the Problem?
Almost everyone involved in health care will tell you that the greatest problem in our system is that we pay on a fee-for-service basis. Almost everyone is wrong.
The logic is obvious – paying a fee for a service encourages providers to get more fees by providing more services. Ergo, we consume too much and spend too much. Ipso facto, getting rid of fee-for-service would result in fewer services and less spending. Case closed.
Well, maybe not.
In fact, almost everything we do in the course of our economic lives, we do on a fee-for-service basis. When we go to the movies, get our oil changed, have our roof replaced, buy a computer, get a haircut, hire a baby sitter, buy a steak dinner, get someone to do our taxes or defend us in a suit, we do it on a fee-for-service basis. None of it is particularly inflationary.
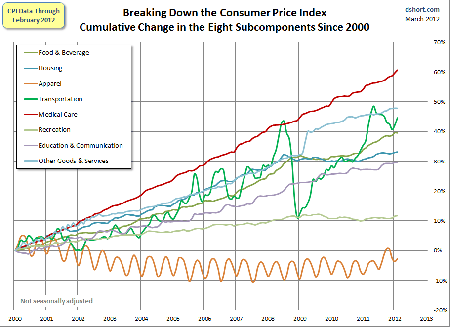
The graph below shows the CPI broken into components. Food, housing transportation, apparel – all are paid fee-for-service and all have a lower rate of inflation than health care.
Yes, the providers of these services would like to sell us more units of service. But we have good reason to resist – we don’t want to waste our money on services we don’t need.
What is unique about health care is not fee-for-service, but third-party payment. Only in health care is there someone else picking up the tab for our spending.
If we applied the same third-party payment technique to any other segment of the economy we would get the exact same inflationary spiral we see in health care. I buy donuts from time-to-time. If those donuts were free at the point of purchase, I would buy (and eat) a whole lot more than I do today. The stereotype of cops eating donuts came about because the donut shops gave them away to the cops for free.
When I was working as a state-level lobbyist for the Blue Cross Blue Shield Association, I would attend meetings of the National Association of Insurance Commissioners (NAIC), the National Governors Association (NGA), the National Conference of State Legislators (NCSL) and a bunch of other organizations. These groups typically held their meetings in the ritziest hotel in Kansas City, New Orleans, San Diego, Boston or some other place that was easy to get to.
Never, not once, did I ever inquire what the room would cost when I checked in. Why should I? Blue Cross was paying for it. The cost made no difference to me whatsoever. Some years later when I went into business for myself and tried to attend the same meetings at my own expense, I became very interested in the cost of the rooms. Most of the time, I would stay at a cheap motel on the edge of town and drive to the meetings.
Ah, but health care is different, you might say. Yes it is. It is different because of third-party payment and for no other reason. The other reasons usually given are easily rebutted –
- Information asymmetry (the providers know more than the patients). Of course, but that is also true of, say, criminal law or engineering.
- Health care is essential to life. But it is far less essential than food or housing, which do not require third-party payment.
- Patients are too fearful to make rational decisions. More fearful than if I were arrested and locked up at Riker’s Island?
- Health care is complicated. As complicated as an iPad? I don’t think so.
Efforts to move away from fee-for-services or to control it never work very well. Witness capitation under managed care, or the RBRVS system of paying physicians under Medicare. Medicare’s system of price controls leads to absurd complexity yet does not reward physicians for the things that are most important to patients, such as kindness, patience, communication ability, friendliness – the qualities that humanize the medical transaction and that would be rewarded in any other segment of the economy not dominated by bloodless third-party payers.
It is about to get worse with the advent of the ICD-10 codebook. This will offer 140,000 separate billing codes, according to The Wall Street Journal, including “codes for injuries in opera houses, art galleries, squash courts, and nine locations in and around a mobile home, from the bathroom to the bedroom.”
It is not fee-for-service that is the problem, but the burden third-party payers put on patients and providers alike, without adding any value whatsoever.


The managed care model attempted to pay “providers” to NOT provide services, and to punish them economically if they referred you to a specialist. It ended up costing a lot more for less services.
Regarding ICD-10, the AMA is fighting it. They currently earn $72 million a year on CPT codes, and perhaps they worry about losing that revenue, since it is more revenue than they receive from dues paying members.
What I like about ICD-10, is that there are 29 billing codes for an injury from a chicken, and because I have chickens, I think it is very important for a doctors and the government to know exactly how a chicken injures me before I am provided with medical care. Frankly, I wonder how doctors ever survived without this system!
Greg – well written and great points. I have been saying for sometime at actuarial meetings and other industry confabs that fee for service has essentially gotten a “bad rap.” The thing is, no matter what kind of global, episodic, or full capitation payment structure might be offered by an HMO, ASO, or medical home arrangement, behind the scenes is a bean counter who is cross checking the number of units used against what was budgeted, in each case multiplied by a unit cost to arrive at the bundled amount. It’s not the service, it’s how much gets used, and the motivations that lie behind that utilization.
Injuries in opera houses! ROTFL!
I agree that fee-for-service does not get to the root of the problem. The real problem is that patients –who are the consumers of medical services –aren’t the ones paying the fees for the services. If patients paid more of their own medical bills directly, providers charging the fees (for their services) would package, bundle and differentiate their products in innovative, patient-pleasing ways and compete on both price and quality.
Most services sold are sold on a fee-for-service basis. Consider food eaten away from home. You can choose from fast food, casual dining and fine dining. Fast food restaurants charge by the item but offer package deals on combo meals. Casual dining generally offers a range of choices at different prices, while fine dining often has multiple choice meals or fixed price meals where you choose your menu items.
Why does this work in the food industry but not in the health care industry? The first observation is that patients are not price sensitive, so providers have less reason to differentiate services. But another reason is the bureaucracy involved when third parties are paying the bill. What has evolved to make third-party payment work is a system of diagnosis related groups and CPT (billing) codes. A hospital isn’t likely to deviate from the established billing codes to package a set of services because it makes the likelihood of getting paid less certain. Also, why would a hospital create a package deal when they make more money charging for each service? Imagine eating at a restaurant and finding the prices wary widely (i.e. by 3:1 or 4:1) from one restaurant to anther for the same quality. Imagine the menu having artificial prices and the actual price paid is different for each customer depending on who is their nutrition insurance company. Imagine being charged separately for dishwashing and for the waiter; each time the waiter asked “is everything is OK?” would result in an additional charge. There would be a separate charge for taking your order – another one for a dietitian to assess if you’re hungry and what your dietary needs are. There would be a table charge, a linen charge, and another for the plates, glassware and utensils. This sounds ridiculous but really isn’t. It’s the way a system would evolve in the absence of consumers paying their own bills.
One other advantage to fees is that the coming payment technology for out-of-pocket medical care will be based more on fees. For instance, if 25% of office visits and biometric tests are done at home, they will be tracked using fees and often paid for more like iTunes, a fee-based music distribution that resembles home self-care. This in effect downstreams the fee-for-service system from the doctor’s office to the home, retail clinic and employer site of care. Global payments freeze in one site of care.
In everyone of your upfront examples the consumer understands (or could easily) the total cost of the episode (babysitter, dinner, haircut, computer purchase, etc.) In the case of roof repair you know the cost of the roof repair itself – if something else is discovered as a root cause the contractor will come back to you with the information and you will get an estimate for that repair.
My point is, that fee for service is not all bad, nor all good. Shots, physicals, eye exams are all great uses for fee for service. But a heart transplant, diabetes care those are different.
When you go to the car dealer you don’t buy all the automobile components and assemble them yourself – you buy the entire automobile, assembled. That’s how you should be able to purchase certain elements of health care.
Great piece Greg. It brings to mind this quote:
“If you tell a lie big enough and keep repeating it, people will eventually come to believe it. The lie can be maintained only for such time as the State can shield the people from the political, economic and/or military consequences of the lie. It thus becomes vitally important for the State to use all of its powers to repress dissent, for the truth is the mortal enemy of the lie, and thus by extension, the truth is the greatest enemy of the State.”
This quote is attributed to Joseph Goebbels, and it seems its message has not been lost on the Statists who seek to control the healthcare industry in this country. How many times have we heard the mantras “Fee for service is the cause of healthcare problems” or “50 million people in the U.S. have no insurance (and thereby no access to healthcare)”?
These and other dubious claims are generally accepted by the great unwashed as factual, and the debate starts there. Consequently we get “garbage in” and “garbage out”, and in this case the “garbage out” is Obamacare.
All forms of insurance create moral hazard See, eg, communism.
My question: since a significant amount of insurance is desired by consumers to protect against large and unanticipated expenditures, and since providers and consumers will in the more extreme cases spend to forestall death, what alternative strategies could the insurer employ to minimize the resulting moral hazard?
John,
This is a masterpiece! Short, simple, easy to understand and a dynamite graphic to boot. I will circulate widely.
michael
Hopefully you do not bank all your conclusions on a single limited, non-scientific, non-statistically significant, geographically and practice limited outcome study. FFS does provide the opportunity for physicians to drive up costs with follow up visits, labs, X-rays, injections and outpatient surgeries that may not be needed or marginally reasonable clinical practice. An orthopedic surgery that has a 50% chance of improving mobility while no surgery has the other 50% chance of achieving the same outcome will more frequently be recommended unless the patient has the knowledge to ask outcome questions. For most consumer a physician is a deity so if they can marginally afford it they will do what the physician recommends expecting that it will always be the best clinical and economical advice.
FFS is not all bad but definitely not the silver bullet. I used to purchase $4B/yr in healthcare and never found the perfect solution. The consumer needs to have some skin in the game but more importantly needs to become health and health care literate to make informed purchasing decisions.
Jon,
Keep in mind the difference between insurance and third-party payment. Yes, insurance induces moral hazard, but third-party payment (TPP) adds exponentially to that problem. Imagine a life insurance contract that operated on the TPP basis. Instead of paying your widow $300,000 upon your death, it would pay the people that provide her with services — the mortgage company, the grocery store, the gas station. She would never know how much was paid on her behalf. The life insurance company would try to manage her care and deny payment for things it thought were not necessary. I may have to expand on this in the future.
I think Jon Kessler is correct in his assessment of “insurance” as a collectivist but necessary concept. The key to its successful application is to apply it properly. “Moral hazard” is best avoided when insurance is only used to shift the cost of “unpredictable risks”. Its current gross misapplication in the health insurance world is one of the primary problems with the healthcare system.
The message in Curmudgeon’s last sentence should be the basis for reforming the healthcare industry.
Greg, this is quite simply the Occam’s razor of the health care financing argument–I wish the Supreme Court had it plasterd to their faces at the end of today’s proceedings!
Don’t forget the other driver of cost and inefficiecy: regulation and cartelization. As a real live regulated cartel member, i know of what I speak!
I take some comfort from the idea that the Court (or to be precise its swing voters) do intact understand exactly the question they must address: is healthcare different? My only concern is they might say, “yes.”
John:
Your post is a home run. One reason why I like a voucher system so much is that it will drive most individuals (perhaps even all) to buy policies that are fee-for-service in structure (in most cases, outright catastrophic plans). This will produce an almost unfathomable improvement in static and dynamic incentives. Because the health care industry has strayed so far from being a free market endeavor, this will produce an almost immediate revolution for the better. The reason why this argument has so much trouble gaining traction is that while central planners can tell you exactly what they are going to do (and inappropriately promise an outcome), the free market never tells you how problems will be solved. Being risk averse and suspicious of corporations, people naturally gravitate to the specifics that government provides. Fee-for-service is better but precisely how it is better can only be demonstrated vis-à-vis indirect logic, and that’s the rub.
David C. Rose
Professor and Chair
Department of Economics
University of Missouri-St. Louis
St. Louis, Missouri 63121-4400
314-516-5550 (phone)
314-516-5352 (fax)
Outstanding example Greg, thanks
Comment; What a great article. Just common sense. But big insurance and Big Government have huge stakes in this.
Is this the protection racket revisited; pay us or suffer the consequences? John Goodman’s unique capacity for uncommon sense shines through again. It’s a cash and carry, consumer oriented solution versus “Bread and Circuses”
After storm damage, my house repairs are paid for by a third-party. If my car is damaged, the third-party insurer covers the repairs. They watch my spending choices like a hawk. The home repair and auto repair industries haven’t created a similar price spiral. Healthcare is not just paid for by a third party, but it’s funded by an employer (in many cases) who gets to deduct the cost from their taxes, and they’re not allowed to control my choices to the same extent as my insurance companies.
L. Brody, you are 100% correct that John Goodman’s penchant for getting to the core of the problems and presenting logical solutions is “uncommon sense”. In this case it is Greg Scandlen who seems to have earned that same kudo.
I owe an apology to Greg Scandlen for not crediting him for today’s Goodman Health Policy Blog. I credited John Goodman, but in general I credit both for being on top of all health care financing issues.
If government does it, you pay for the bureaucracy indefinitely through its permanance. If you have any doctor to patient or hospital to patient payment, you eliminate a lot of middle men.
I thank Frank Timmins above for correcting my error
L. Brody
@Curmudgeon,
How could you expect to find a “silver bullet” for $4B/year in health spending? (Were you running the VA? Or is the “B” a typo?) Sure, the doctor has an incentive to order another test. So does the car dealer have the incentive to sell me a Lexus, but I bouught a Prius because I saw the price difference.
@Rich Stenner,
You write that after a storm or auto accident, the insurer watches your spending like a hawk. However, they are price takers, not price setters, of the goods and services. All the components of your home and car were originally supplied in a normal market, so everyone knows what the correct price is. In health care nobody knows what the correct price is – certainly not the third-party payers!
Mr. Brody,
No apology required. I could do a lot worse than being confused with John Goodman.
To build on my erstwhile Canadian friend Mr. Graham’s comment, it is circular reasoning: because there is no functioning market we don’t have price transparency so a functioning market can’t work. We have markets for food, water, shelter and energy, all of which I would note are cheaper, more plentiful and safer in the United States than almost anywhere in the world. But apparently only by government mandate can our country be made safe for erectile disfunction treatments, birth control pills and other “minimum essential coverage.”
Healthcare is different!
@Jon,
We are building a market at http://www.MediBid.com and it does work. We introduce price transparency, and competition and it works. I know that your last line is said with tongue is cheek, but markets work in healthcare
John,
When will you learn that getting a haircut or going grocery shopping cannot and should not be equated with paying for health care. I am firmly believe that fee for service should be the preferred method of paying for all office visits. The way it is now is that the insurance companies determine which doctors you can see, what hospitals you can go to, what tests you may have and what medicines you can take. High deductible, lower cost policies should be the model as it was 30-40 years ago. Then if doctors try to add more revenue generating studies, tests, then monitoring these parameters should become part of a doctor’s report card. One cannot increase revenue by denying services, the only way is to give the doctor enough time to adequately assess a patients complaints, do what is necessary and be included in the specialty areas as being “better”, and then let the doctors slug it out. Overcharging, utilizing equipment which if used excessively will show up on a national registry to receive a score. If one does a better job, gives a thorough physical exam, and orders all appropriate therapy, this will provide an equitable way to assess performance and reimburse the doctor from these parameters. Sucess of the health care mess is to take it out of the realm of fiscal curtailment, then we can have a return to what we were all trained to do. If a doctor can have enough time to take a complete history. do a complete physical, and then order studies to help him make a diagnosis (which can be achieved 80% of the time) rather than rely on studies, x-rays, and other expensive tests before the patient has been evaluated only serves to increase costs. One example that happened to me; went to the hospital, complained of chest pain, and I was immediately considered a cardiac patient. I then had a chest xray EKG, CT, blood gases and then, after $3500, the doctor arrived to do a physical; Would you believe that I had a plural effusion in my right chest which could have been easily diagnosed from my history and physical findings. All for less that $300. That’s all for now.
Dr Bob Kramer
214 676 5692 office
214 522 8040 fax
drbobkramer@pol.net
Dear John
One thing that has been missing from the analogy between health and auto insurance is that the states may or may not enforce the auto insurance requirement. So, in my case, we’ve had a supplemental item called, “Uninsured Motorist.” What hospitals and other providers need is something like this – called Uninsured patients. Either that, or we should require the states to allow us to buy our auto insurance when we have an actual need such as an accident.
Sincerely,
Glenn Smith
Mr. Smith.
That’s a fine idea. It is interesting that even with a mandate, the rate of non-insurance in auto is about the same as it is in health. In health we did develop a “residual market” in the form of high risk pools. They have worked pretty well, though underfunded in most states. It would have been far better if the Feds had simply helped pay for risk pool losses.
Dr. Kramer,
It sounds like you are arguing for “concierge medicine.” It is interesting that this is the only area I can think of where “capitation” actually works well. Perhaps it is because the capitated payment comes directly from the patient, not a third-party payer.
“But we have good reason to resist – we don’t want to waste our money on services we don’t need.”
already a false premise: WE do not make the decision to get an MRI, EKG, etc. the PROVIDER of the care (also the biller) does. AND, we are NOT wasting OUR money, we ARE wasting insurance co/govt (see medicare/medicaid) money. Geeze
Mr. Hooker,
That is precisely the point. We don’t mind wasting other people’s money.
Greg: Pointing out common sense to those without common sense can certainly feel like pushing water uphill.
In the mind set of those that can’t see the obvious rationale you so well describe, health care is not a service, but a “right” that all should have access to for free. Intellectually they reject personal financial responsibility, and thus rational arguments based on free market principles fall on deaf ears.
A free market with financially responsible health care consumers versus equal access to free health care for all, thru a centrally controlled government-run entity are diametrically opposite goals.
Since the subject is so deeply steeped in partisan ideology, I suspect it will only be solved by brut political force; not cogent analysis of the facts…
In 1954 health plans became taz deductible. This shifter growth in funding away from wages, and towards healthcare, which in part is responsible for the difference
I’ll tell you what the silver bullet is, that John Graham is looking for: If doctors and hospitals would stop billing insurance all together, and they dealt directly with patients, cut out mandates from “health insurance” policies, we would see costs drop tremendously. Who was it that decided doctors should bill insurance, anyway?
The problem is that healthcare is paid with Other Peoples Money. Most people dont purchase health insurance iwth their own money and even if they do they are insulated from actual coast. If persons had to pay for services as they undertook them spending woudl be far more careful. this problem of spending other peoples money is the problem with big government . government spends other peopels money. Most pts spend other peoples money. Threat of litigation results in many more tests ordered than might be done if threat did not exist. Obamacare will increase not decrease demand and will lower payment to pay for it. They can only go so low. Nurses and ancillary staff will take over much of role of physicians. Ultimately litigation crisis may end when it is government that has to pay the litigation costs when we all eventually become government employees and government is on the hook. Govnt however will try to insulate themselves from such liability via indep contract type language but ultimately we will defacto be working for the govnt in one way or another.
Dont’ have much time to write a long note,…but a few thoughts seems to ring out at this moment, having read the above.
GREED…. at all points of the compass.
Expectations….beyond reasonable, from all parties.
Entitlement mentality at all levels…both public assistance and the insured. Hey, even providers have an entitlement mentality!
When we have to be a part of the payment, our choices are affected!
When it’s cheap / covered / free….we make different decisions than we would otherwise. FACT.
Finally, providers run toward the “prodecures”! FACT. Why…? MONEY. Don’t lie. It’s the truth and we know it.
The whole system is broken and everyone’s pointing the figure away from themselves. 🙂 What’s new?
We all need to do our part to see that things get turned around, but most of us have no real place at the decision-making table.
It’s all being shoved down our throats….due to the fact that the powers that be control…yep, you guessed it, the money!
Sad situation.
I was happiest in medicine when I had a totally cash practice. Then 2008 came along.
The ICD-10 has caught me totally off guard. How many clerks will it take to look up a diagnosis code? Will I get paid more if the patient gets injured at an opera than at a trailer park?