Unconnected Medical Devices Harm Patients
The federal government’s dominance of health information Technology (HIT) has been most apparent, and most harmful, in electronic health records (EHRs). However, the hand of government must lie heavily in other parts of health care, too.
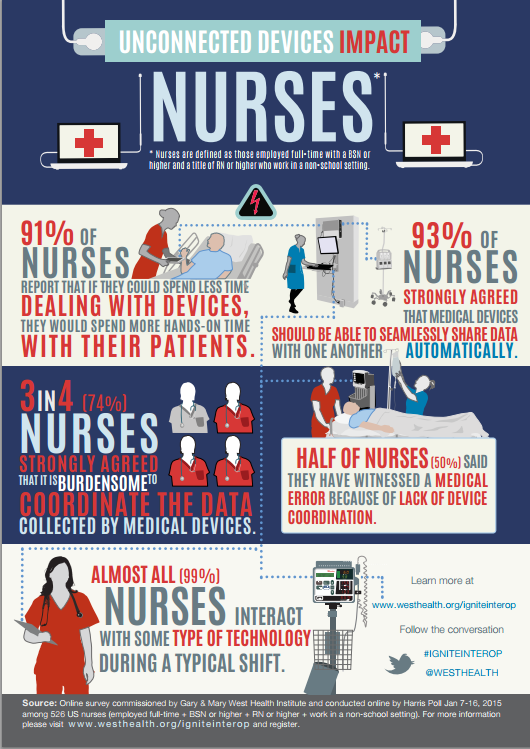
An example is medical devices hooked up to patients at the hospital. Remarkably, these devices do not talk to each other, requiring nurses to waste time transcribing data from one device to another. This infographic summarizes a survey of 500 nurses commissioned by the West Health Institute:
These are appalling figures. I don’t know about you, but I figured out how to connect my VCR to my TV sometime during the 1980s. Medical devices are heavily regulated by the FDA. The fact that devices critical to hospital patients’ health are still not connected strikes me as a likely consequence of over-regulation.